Impact analysis in IEHIAS
- The text on this page is taken from an equivalent page of the IEHIAS-project.
The results of an environmental health impact assessment can be presented in a wide variety of ways, and which is most appropriate will depend on the purpose of the analysis and needs of the users. Ideally, the indicators to be used will have been identified at the Issue framing stage (see Selecting indicators in IEHIAS), and further specified if necessary during Design of the assessment. These indicators can be targetted at any point in the chain between source and health outcome, according to need (see Selecting indicators in IEHIAS#Position in the causal chain). The number of outcome indicators may also vary, depending on the complexity of the issue being addressed and the interests of stakeholders. In most cases, however, they will include one or more synoptic endpoint indicators, summarising the health-related impacts at a collective level.
Construction of these summary measures is known as impact analysis. The process is inevitably one of averaging and aggregation, for most issues subjected to an integrated assessment involve a number of different health effects, varying in their physiological characteristics, severity, duration and wider implications (e.g. in terms of mobility, social stigma). Like all such summary measures, they thus imply some loss of information, and may hide many of the subtleties and variations of effect, and their causal relationships. For these reasons, they need to be defined and used with care. They nevertheless add value to an assessment by making the results both more generalisable and more usable in policy terms. They provide, for example, a basis for:
- Comparative evaluation of environmental problems and health impacts (“how bad is it?”)
- Attribution of overall impacts between different sources and causes (attributable burden of disease)
- Quantification of the overall health impact of policies or technologies ("what unintended health impacts might it cause?")
- Evaluation of the overall effectiveness of environmental or health policies (largest reduction of disease burden)
- Communication of health risks and impacts
Types of impact measure
A range of different impact measures can be constructed and several are widely used. These include measures based on:
- mortality - e.g. total mortality, life expectancy, years of life lost (YLL);
- morbidity - e.g. limiting long-term illness (LLTI), years lived with disability (YLD);
- a combined disability-weighted measure of health - e.g. disability-adjusted life years (DALYs), quality-adjusted life years (combination of mortality and morbidity;
- monetary values - e.g. monetary cost, monetary benefit, net monetary value.
Each of these represents the use of a somewhat different 'measurement construct', and reflects different underlying value systems. For example, total mortality implies that death is the (only) relevant outcome, and that all deaths are equal; years lived with disability (YLD) focuses on the duration of the effect but not (beyond the threshold needed to classify as disabled) its severity; monetary measures are based on the assumption that all health impacts have definable financial equivalents, and that economic value is a valid basis for comparison. Because these underlying principles may not be shared (or fully understood) by all users of the assessment results, care is needed both in using and communicating these impact measures. In many instances, it may be useful to apply more than one indicator, both to explore whether they produce comparable results, and to satisfy the varying expectations and needs of different stakeholders. The impact measures also need to be clearly explained, in order to aid interpretation.
Key issues in impact analysis
The majority of environmental processes and agents that affect human health are not singular in their effects, but cause or contribute to a range of different health outcomes. Atmospheric particulates, for example, are implicated in a range of illnesses, including upper and lower respiratory tract infections, cardivascular diseases and cancers. Exposure to noise may impair learning abilities, cause sleep disturbance and annoyance, and contribute to raised blood pressure and cardiovascular illness. These various effects may also manifest themselves differently between different individuals (and in one individual over time), depending on the level of exposure, the susceptibility of the people concerned, and the course of the illness. Health effects are therefore both varied and multivariate phenomena. Combining them into a single, interpretable measure of impact is not always easy.
Five sets of factors, in particular, have to be considered and allowed for in devising and applying measures of impact:
- Type of effect. The majority of environmental processes and agents that affect human health are not singular in their effects, but cause or contribute to a range of different health outcomes. Air pollution, for example, is implicated in both upper and lower respiratory tract infections, cardivascular diseases and cancers. Nor are the effects necessarily adverse; many policies and other interventions have important positive effects for health - e.g. by providing protection from disease or by enhancing people's physical condition, sense of well-being and quality of life.
- Scale of effect. Any outcome, whether adverse or beneficial, may vary greatly in its degree. Diseases, for example, may vary in their severity from mild discomfort (or concern) through to total incapacity and, ultimately, death. Cases of any disease are therefore not necessarily equal, but need to be weighted in some way to reflect their differing severity. Likewise, beneficial effects may vary in terms of their degree of benefit, from mild alleviation of symptoms through full protection against adverse effects to full enhancement of quality of life.
- Duration of effect. Likewise, diseases may persist for different lengths of time (either as a single period or repeated events). The overall impact of the disease thus has to be considered as the sum of its effects over this entire duration.
- Timing of effect. Health effects may arise at different life-stages, from pre-birth (in utero) to old age, and in some cases, may even be delayed to future generations. Independently of their duration, this may affect people's attitudes to the effects: there is a tendency, for example, to attach higher values to immediate events compared to those that are deferred until later (discounting).
- Target of effect. In addition to the above, the way in which any effect is valued depends on the underlying social priorities of those concerned. These may not be based on simple utilitarian principles, but may give preference to some groups over others (e.g. in the endeavour to maintain or reduce social inequalities). Thus perceived differences in impact may exist depending on who is affected.
Impact analysis thus involves more than simply summing the incidence of disease across different outcomes. It requires the incorporation of, and trades-off with, beneficial effects; and it requires all effects to be weighted according to their scale, duration and timing and the social values that may be attached to different groups of individuals. All impact analyses are thus contextual in that they are rooted within a specific (though often implicit) value system. If the analysis is to be acceptable and meaningful to the users, the value system needs to be made explicit, and should reflect the needs of the users concerned.
Methods and measures for impact analysis
Types of impact measures
A number of different metrics and methods have been devised to evaluate impacts. These are based both on different measurement systems (or 'frameworks of commensuration') and, underlying these, different value systems - for example, the relative importance attached to issues such as social equity, economic effectiveness and individual freedoms.
In the context of environmental health, understandably, the majority have used health-based metrics (see link to Health-based impact measures in panel to left). These derive from measures of the incidence of morbidity and mortality, the simplest comprising counts of the total number of cases of mortality or of people with a specified disease. More sophisticated measures weight these according to duration in some way: e.g. by counting the number of years with the disease, or the years of life lost (relative to a 'normal' lifespan). The most elaborate measures, such as disease-adjusted life years or quality-adjusted life years also weight outcomes according to severity (see link to DALYS and QALYs, below).
In recent years, however, monetary measures of impact have also been applied (see link to Monetisation methods, in panel to left). These involve the estimation of the monetary value of health benefits and the costs of adverse effects, not only in terms of the more obvious and tangible costs of health care and lost productivity, but also relatively intangible costs such as reduced quality of life. Although relatively complex in their formulation, they tend to be favoured both because they are, for many users, more intuitive and (apparently) readily understandable than health-based metrics, and because they are more directly relevant to policy decisions, in which cost-efficiency or cost-effectiveness are often crucial considerations. Because they are expressed in terms of a more generally applicable measurement system, they also facilitate the comparison of health impacts with other potential considerations, such as environmental or economic impacts. Monetary measures may also be explicitly linked to health-based metrics, for example by calculating the cost per DALY (or QALY) as a measure of policy effectiveness.
A generic framework for impact analysis
Impact analysis can be seen as the attempt to combine different health outcomes, into a single, synoptic measure of health impact, on the basis of a consistent measurement scale. As the summary above indicates, however, health outcomes vary not only in their form (i.e. type of disease), but also in their severity (from mild symptoms ultimately to death), duration and timing. Health effects may also arise at different times, either more or less immediately, and their timing may affect the value placed upon them (since people would often prefer to defer illness for as long as possible). In addition, the question often arises as to whether everyone is equal in terms of the implications of health effects: susceptible (under-priveleged) groups might be considered to suffer more, for example, because of their inability to pay for treatment or otherwise ameliorate the health effects.
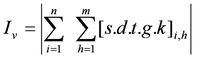
These different factors are not always considered explicitly in impact analysis, and where they are considered may be dealt with somewhat differently. Nevertheless, they are certainly implicit in every measure of impact. Generically, therefore, impact analysis can be expressed as follows:
where: Iv is the overall health impact (in the context of value system v);
i specifies the individual (or sub-group of individuals) affected;
h specifies the health outcome;
s is the weight for the scale (e.g. severity) of health effect h in individual (or sub-group) i;
d is the weight for the duration of health effect h in individual (or sub-group) i;
t is the discount factor, applied to the timing of the health effect h in individual (or sub-group) i;
g is a weight for an effect in the population group to which individual or sub-group i belongs
k is a scaling factor, to convert the impacts into the relevant measurement units (e.g. cost of standard life).
This equation thus forms the framework for all impact analyses, and it is often informative when considering different measures to identify clearly which of these factors are allowed for (i.e. by some form of weighting) and which are ignored (and given, by default, a weighting of 1).
Health-based impact measures
A range of aggregate health metrics have been devised for use in assessing policy impacts or the effectiveness of health management systems. Many are also used as indicators for routine monitoring of health status at the national or international level. A number are summarised below.
| Acronym | Description | Definition |
|---|---|---|
| LE | Life expectancy | Average number of years a new-born baby would survive, were he or she to experience the particular area's age-specific mortality rates for that time period throughout his or her life. |
| HLY | Healthy life years | Number of remaining years that a person of a certain age can be expected to live without disability. |
| YLL | Years of life lost | Total number of years of reduced life due to premature mortality: calculated as the number of deaths multiplied by a standard life expectancy at the age at which death occurs. |
| LLTI | Limiting long-term illness | Number of people affected by long-term illness, health problem or handicap which limits the daily activities or the work that a person can do. |
| YLD | Years living with disability | Number of years lived with a specified disease. |
| DALY | Disability adjusted life years | The sum of years of potential life lost due to premature mortality and the years of productive life lost due to disability. |
| QALY | Quality adjusted life years | How many extra months or years of life of a reasonable quality a person might gain as a result of treatment (particularly important when considering treatments for chronic conditions). |
Each of these measures may be useful in specific circumstances (e.g. depending on the range of health effects of intrest). DALYs, however, are generally the most relevant for integrated environmental health impact assessments, because they bring together, within a single measure, both morbidity and mortality effects, and take explicit account of both the duration and severity of morbidity and the timing of mortality (see link to QALYs and DALYs, below). Calculation of many of these measures can also be relatively complex, because of the need to estimate long-term effects, and to make allowance for underlying trends in life expectancy in the population. A calculation tool is therefore provided via the link below, which computes DALYs and several other key health impact measures .
See also
- Selecting indicators in IEHIAS #DALYs and QALYs
- Impact calculation tool
- Calculating DALYs: waste
- Calculating DALYs: UVR and skin cancer
- Impact analysis: transport