Health effects of benzene in Europe
| This page is a product of the EBoDE project. The final report of the EBoDE project has been published as a report in 2011[1] and also as web pages in Opasnet. These links lead to parts of the report.
EBoDE project: main page | overview | contributors | data overview | Parma meeting | abbreviations | all pages Methods: environmental burden of disease calculation | selection of exposures and health effects | data needed | impact calculation tool Health effects in Europe: benzene | dioxins | formaldehyde | lead | ozone | particulate matter | radon | second-hand smoke | transport noise | environmental burden of disease | results by country |
This page is a study.
The page identifier is Op_en5202 |
|---|
| Moderator:Mori (see all) |
|
|
| Upload data
|
Benzene
About benzene
Benzene is an organic chemical compound that was added to gasoline in the past. The use of benzene as an additive in gasoline is now limited, but it is still used by industry in the production of for example drugs and plastics. In addition, cigarette smoke contains some benzene.
Inhalation is the major route of human exposure to benzene. However, exposure may also occur through oral absorption or by dermal exposure (primarily in workplace settings). Exposure to benzene- contaminated water can cause inhalation and dermal absorption in the general population (e.g. when having a shower), but this does not occur often (US Department of Health, 2007).
The genotoxicity of benzene has been extensively studied. Benzene is a known carcinogen for which no safe level of exposure can be recommended. The most significant adverse effects from prolonged exposure to benzene are haematotoxicity, genotoxicity and carcinogenicity (IARC group 1 carcinogen) (IARC 1982, 1987). Chronic benzene exposure can result in bone marrow depression expressed as leukopenia, anaemia and/or thrombocytopenia, which can in turn lead to pancytopenia and aplastic anaemia (WHO, 2000b). Increased mortality from leukaemia has repeatedly been demonstrated in workers occupationally exposed (Arp et al 1983, IARC 1982, Decouflé et al 1983, Bond et al 1986, McCraw, 1985, Yin 1987, Paxton et al. 1994a, b). There are also studies that using proxies of benzene exposure indicate an increased risk of leukaemia in children, but conclusions are not definitive (Weng et al, 2009, Brosselin et al, 2009, Whitworth et al 2008, Gunier et al 2008, Steffen et al, 2004, Crosignani et al, 2004, Pearson et al, 2000, Nordlinder et al, 1997).
Benzene was selected in the EBoDE project because it may pose high individual risks and is still of global concern. Even though policies in Europe have already greatly reduced environmental benzene exposure, it is still identified as a concern (e.g. the INDEX project identified benzene as high priority stressor (Koistinen et al., 2008, Kotzias et al., 2005); European air quality directive 2008/50/EC; setting of WHO guidelines for indoor air quality (WHO, 2010b)). [1]
Selected health endpoints and exposure-response functions
Benzene effects were estimated for leukaemia, including morbidity and mortality. Other proposed health endpoints were not included, because they only occur at high exposure levels, typical of occupational settings. We used the exposure response function as recommended by the WHO Air Quality Guidelines (WHO, 2000b) (see Table 3-19 in section 3.12). WHO uses the 1984 risk calculation of Crump (1984), in which the geometric mean of the range of estimates of the excess lifetime risk of leukaemia at an air concentration of 1 µg/m3 is estimated to be 6 × 10-6 (unit risk). This estimate falls within the range of the risk estimate that is used by the US EPA (2.2 x 10-6 to 7.8 x 10-6 per µg m-3). This unit risk is applied to the whole population, including children. Specific estimates that have been supplied for children could not be used, because the underlying studies often use proxies of exposure (petrol station density, traffic density, etc.) instead of actual benzene exposure levels.
The estimated number of leukaemia cases were used to calculate the population attributable fraction using method 2A. [1]
Exposure data
Benzene exposures are best described by residential indoor air levels (µg m-3). Besides being affected by benzene levels in outdoor air, indoor levels may be raised especially by indoor smoking and potentially the storage and use of fuels e.g. in case of attached garages and storage rooms.
Benzene is a regulated ambient pollutant and therefore outdoor monitoring is required by the European Union. Benzene measurements are included in the AirBase database (European Environment Agency, AirBase, 2009).
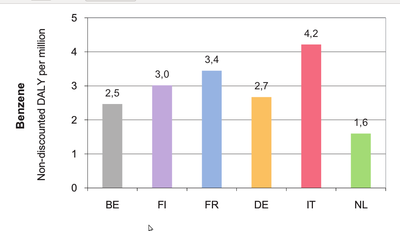
Benzene exposure is estimated from national indoor levels, supplemented with outdoor levels. Different national data demonstrate that benzene exposure concentrations vary from 0.9 µg m-3 in the Netherlands to 2.9 µg m-3 in Italy. The data used in this project are summarized in Table 3-21 in section 3.12.
The confidence levels of the exposure data cannot be directly compared, because the measurements are based on different time periods. Data from the Netherlands and France reflect a 1 week average exposure, while Italian and Finnish data are based on 2 day measurements.
Sources of uncertainty in exposure data include differences in sampling selection. In France, data reflect a large number of dwellings, while in other countries data are limited to a smaller number of monitored houses. In addition, the presence or absence of tobacco smoke in indoor environments is not always reported, making comparison more difficult. This at least partly explains the higher levels in Finland, where benzene from smoking was included. In Italy, levels are likely to be higher because of the large number of two-stroke engines used there, which emit a lot of benzene. [1]
| Country | Including benzene from smoking | Sample size | Time periods of measurements |
|---|---|---|---|
| Belgium | Yes | 85 houses and 25 day-care centers | |
| Finland | Yes | random; 20 adults | 2 day average |
| France | Yes | 567 residences | 1 week average |
| Germany | Yes | 1790 subjects | |
| Italy | Yes | 50 subjects | 2 day average |
| Netherlands | Yes | 1240 dwellings | 1 week average |
Uncertainties per stressor and comparison with other studies
A list of the most important sources of uncertainty for each stressor in the EBoDE calculations is provided in Table 5-1. Some of these are further explained below. In addition, we will compare our estimates to results of a selection of similar studies. Comparison of different studies on environmental burden of disease helps to understand the role of various methodological and strategic selections made in each study, like the selection of stressors or health endpoints.
Benzene No international burden of disease study utilizing DALYs for benzene was identified. Some studies using exposure proxies like proximity of gasoline stations have studies health impacts with inconsistent results. Dioxins. Our calculations were based on the same approach as applied earlier by Leino et al (2008), but we utilized an updated cancer slope factor that is approximately seven times higher than the one used by Leino et al. Leino et al. did the calculations for Finland only. The work presented here also updated the exposure estimates in order to allow for good international comparability, yet some differences between the national intake estimation methods remained. [1]
| Excluded health endpoints and related assumptions | Exposure data | Exposure response function | Calculation method | Level of overall uncertainty a) | Likely over- or underestimation b) | |
| Benzene | Anaemia; genotoxicity; other blood cancers than leukaemia; leukaemia morbidity; effects on the immune, endocrine and nervous system; acute effects. All cases of leukaemia assumed to be fatal | Population representativity varies. Differences in number of dwellings. Different types of measurements (indoor/outdoor; in – or excluding SHS, etc). Sampling times differ | No specific relationships for children used (i.e. same UR used for all ages) | UR method of calculating PAF leads to overestimation because all cases are assumed to be fatal. | * | Underestimation due to excluded health endpoints, but overestimation due to UR method |
References
- ↑ 1.0 1.1 1.2 1.3 1.4 Otto Hänninen, Anne Knol: European Perspectives on Environmental Burden of Disease: Esimates for Nine Stressors in Six European Countries,
Authors and National Institute for Health and Welfare (THL), Report 1/2011 [1] [2] Cite error: Invalid
<ref>tag; name "EBoDe" defined multiple times with different content