Health effects of Second-hand smoke in Europe: Difference between revisions
(Template:ebode added) |
|||
| Line 1: | Line 1: | ||
{{ebode}} | |||
{{study|moderator=Mori|stub=Yes}} | {{study|moderator=Mori|stub=Yes}} | ||
[[category:EBoDE]] | [[category:EBoDE]] | ||
Latest revision as of 14:12, 19 November 2012
| This page is a product of the EBoDE project. The final report of the EBoDE project has been published as a report in 2011[1] and also as web pages in Opasnet. These links lead to parts of the report.
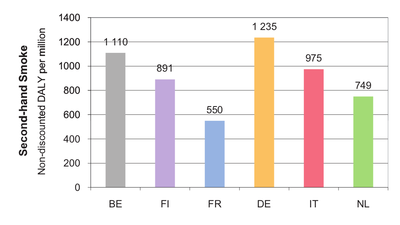
EBoDE project: main page | overview | contributors | data overview | Parma meeting | abbreviations | all pages Methods: environmental burden of disease calculation | selection of exposures and health effects | data needed | impact calculation tool Health effects in Europe: benzene | dioxins | formaldehyde | lead | ozone | particulate matter | radon | second-hand smoke | transport noise | environmental burden of disease | results by country |
This page is a study.
The page identifier is Op_en5204 |
|---|
| Moderator:Mori (see all) |
| This page is a stub. You may improve it into a full page. |
| Upload data
|
Second-hand smoke
About second-hand smoke
Second-hand smoke (SHS; also called environmental tobacco smoke or passive smoking) is a known human carcinogen (IARC, 2004). Exposure to SHS has been shown to cause lung cancer, IHD (ischemic heart disease) sudden infant death syndrome, asthma, lower respiratory infections in young children, low birth weight, reduced pulmonary function among children, acute otitis media, and acute irritant symptoms (WHO, 1999; Californian EPA 2005; US Surgeon General 2006; IARC 2004, Jaakkola et al. 2003). Most evidence for SHS-related impacts is fairly consistent.
SHS has been selected in our study because of its high public health impact, public concern and political interest. Policy measures to (further) reduce SHS exposure have been implemented in the recent past (e.g. the smoking ban) and further policy actions may be taken in the future. [1]
Selected health endpoints and exposure-response functions
Out of the large number of health endpoints that SHS is associated with, we selected mortality and morbidity due to lung cancer and ischemic heart disease (IHD), morbidity due to onset of asthma (both in children and in adults), lower respiratory infections and acute otitis media. For the other health endpoints mentioned above, strong evidence is available, but the necessary disease statistics were lacking.
For the SHS-related burden of disease calculations, we have followed the recent WHO methods on the global estimation of disease burden from SHS (Öberg et al. 2010). A summary of outcomes with their respective evidence levels is provided in Table 3-5. The exposure response functions are presented in Table 3-19.
The selected exposure-response values are not gender-specific (e.g. exposure to male or female smoking spouse; exposure to paternal or maternal smoking). Instead, we used the mean relative risk for exposure to adults’ smoking. This choice was made in order to limit the sensitivity to gender-specific changes in smoking habits over time and across countries, and because not all exposure data were provided separately for men and women.
The selected outcomes are being applied only to non-smokers, i.e. to the non-smoking disease burden. To that effect, the disease burden due to active smoking has been deduced from the total disease burden, by country (based on total disease burden and active smoking disease burden by country provided by WHO; update 2002 based on Ezzati et al. (2004)). [1]
| Health endpoint | Description | Conclusion regarding the level of evidence (in 3 reports) | ||
| WHO (1999) | Californian EPA (2005) | U.S. Surgeon General (2006) | ||
| Outcomes in children | ||||
| Acute lower respiratory infection (ALRI) | Incidence of acute lower respiratory illnesses and hospitalizations | *** | *** | *** |
| Otitis media (middle ear infection) | Incidence of otitis media | *** | *** | *** |
| Asthma onset | Incidence of new cases | n | *** | ** |
| Outcomes in adults | ||||
| Asthma induction | Adult-onset incident asthma | *** | ** | n |
| Lung cancer | Incidence | *** | *** | *** |
| Ischemic heart disease (IHD) | Incidence of any ischemic heart disease | *** | *** | n |
* = The evidence of causality is concluded to be “inconclusive”, “little”, “unclear” or “inadequate”.
** = The evidence of causality is concluded to be “suggestive”, “some” or “may contribute”.
*** = The evidence of causality is concluded to be “sufficient” or “supportive”.
n = Not evaluated in the report.
Exposure data
Exposures to SHS and background risks vary by gender. Therefore, the data collection should account for differences in the exposures by gender. Some health effects are specific for children, so exposure data also had to be collected separately for children. Overall, the following exposure data are required for estimating the health impacts from SHS:
- Percentage of children exposed to SHS (i.e. regularly exposed), OR percentage of children having at least one smoking parent
- Percentage of non-smoking men exposed to SHS
- Percentage of non-smoking women exposed to SHS
For exposure data collection, we used data from national and international surveys as for example the Survey on Tobacco by the Gallup Organization for the European Commission (EC, 2009) or the European Community Respiratory Health Survey (Janson et al. 2006). The fieldwork for this study was conducted in December 2008 and over 26,500 randomly-selected citizens aged 15 years and over were interviewed in the 27 EU Member States and in Norway. The exposures for the six countries included in EBoDE are presented in Table 3-6. The “upper estimate” is used as the most realistic estimate, as this exposure description matches best the exposure definition used in epidemiological studies from which we derived our exposure-response functions. The lower estimates are provided in Table 3-6 for future sensitivity analysis. Table 3-21 in section 3.12 provides a summary of these data. [1]
| Children | Adults | |||||
|---|---|---|---|---|---|---|
| [%] | Data year, reference | men [%] | women [%] | total [%] | Data year, reference | |
| Belgium a) | - | - | 59 34 - |
48 32 - |
53 33 25/30b) |
1990–1994, ECHRS I1 2002, ECRHS II1 2008, Eurobarometer2c) |
| Finland | 7 | 1996, Lund3 | 14 - - |
13 - - |
- 15 6/14b) |
2002, Jousilahti4 2004, NPHI5 2008, Eurobarometer2d) |
| France | 23/33b) | 2005, INPES6 | 38 23 - - |
46 30 - - |
42 26 13/21b) 13/22b) |
1990-1994, ECHRS I1 2002, ECRHS II1 2005, INPES6b) 2008, Eurobarometer2 |
| Germany | 24 | 2003-2006, GerES IV7 |
48 51 28 - |
42 60 26 - |
44 - 27 20/28b) |
1990-1994 ECHRS I1 1998, BGS8 2002, ECRHS II1 2008, Eurobarometer2 |
| Italy | 50 | 2001, ICONA9 |
62 37 - |
49 30 - |
55 34 22/26b) |
1990-1994, ECHRS I1 2002, ECRHS II1 2008, Eurobarometer2 |
| Netherlands | 20/36b) | 2000-2005, RIVM10e) |
68 - 45 - - |
67 - 33 - - |
67 30 39 18/40b) 18/27b) |
1990-1994, ECHRS I1 1998-2001, RIVM10 2002, ECRHS II1 2004-2007, RIVM10 2008, Eurobarometer2 |
NA: Adequate data not available
NB: Additional national data are available for some countries, however, these did not match the description of regular exposure.
Definitions used for lower and upper estimates:
a) For Belgium, no data for children was found; estimate is calculated using mean of other countries.
References: 1 Janson et al. 2006; 2 EC 2009; 3 Lund et al. 1998; 4 Jousilahti and Helakorpi 2002; 5 Finnish National Public Health Institute, 2004; 6 Institut National de Prévention et d’Education pour la Santé (INPES) 2005; 7 Conrad et al. 2008; 8 Schulze and Lampert 2006; 9 Tominz et al. 2005; 10 van Gelder et al. 2008.
b) Lower/upper estimates; INPES: Lower estimate based on “regular” exposure; upper estimate based on exposure “from time to time”;
Eurobarometer: Lower estimate based on daily exposure of more than one hour exposure at work and home exposure; upper estimate based on daily exposure of also less than one hour at work and home exposure. RIVM: ranges based on values provided by various studies.
c) Exposure at home and at work supposed to be distributed equally.
d) Finnish national data (NPHI) also provide survey results, but total exposure to SHS for non-smokers are more difficult to interpret. Therefore only the Eurobarometer data were taken into account here.
e) The RIVM report contains data from various studies (e.g. Doetinchem, STIVORO, PIAMA)
Available exposure data (Table 3-6) range across several years, and have been assessed with slightly differing
definitions of exposures. In order to estimate exposure data for the target year (2004), exposures have been
modelled on the basis of the survey data listed in Table 3-6 as follows:
- Modelling was performed with total adult data, and men/women and children data were assumed to vary according to the same trends.
- Power functions showed the highest correlations in most countries, and were therefore applied in all
countries. No trend was apparent for Finland, therefore only the mean was applied. [1]
Resulting trends are displayed in Figure 3-1, and estimated exposure data for 2004 in Table 3-7.

FIGURE 3-2. Observed SHS exposure levels (markers) (% of non-smokers) for adults and corresponding modelled trends (lines) in the participating countries.
| Year 2004 | Children | Adults (total) | Women | Men | ||||
|---|---|---|---|---|---|---|---|---|
| Lower* [%] |
Upper* [%] |
Lower* [%] |
Upper* [%] |
Lower* [%] |
Upper* [%] |
Lower* [%] |
Upper* [%] | |
| Belgium | NA | NA | 28 | 32 | 27 | 31 | 29 | 33 |
| Finland | 4 | NA | 14 | 14 | 14 | 14 | 14 | 14 |
| France | 23 | 33 | 17 | 25 | 20 | 29 | 15 | 22 |
| Germany | 24 | NA | 26 | 31 | 25 | 30 | 27 | 33 |
| Italy | 40 | NA | 26 | 30 | 23 | 26 | 29 | 32 |
| Netherlands | 20 | 36 | 22 | 30 | 19 | 25 | 26 | 34 |
* Lower and upper estimates correspond to different computations of survey data. For example, the upper estimate corresponds to the inclusion of shorter durations of exposure from certain surveys.
Uncertainties per stressor and comparison with other studies
A list of the most important sources of uncertainty for each stressor in the EBoDE calculations is provided in Table 5-1. Some of these are further explained below. In addition, we will compare our estimates to results of a selection of similar studies. Comparison of different studies on environmental burden of disease helps to understand the role of various methodological and strategic selections made in each study, like the selection of stressors or health endpoints.
Second hand smoke(SHS):Our burden of disease calculation for SHS was based on a WHO model (Öberg et al., 2010). The exposure estimates were updated against available national and international data sources for the target year 2004, but otherwise the results are comparable with the WHO assessment. Other recent estimates of burden of disease for SHS were also available for Germany (Heidrich et al. 2007; Keil et al. 2005), which provided similar results as the current estimates.[1]
| Excluded health endpoints and related assumptions | Exposure data | Exposure response function | Calculation method | Level of overall uncertainty a) | Likely over- or underestimation b) | |
| Second Hand Smoke | Sudden infant death syndrome; low birth weight; reduced pulmonary function among children; acute irritant symptoms. | Data from different years and consequent temporal interpolation. Differing definitions of exposures. Data gaps for some countries | ERF from earlier decades when questionnaire responses may have been less sensitive. Odds ratios used as RR estimates | Various assumptions made, e.g. smokers are not susceptible to SHS | * | Underestimation due to excluded endpoints. Potential overestimation due to increased questionnaire sensitivity |
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Otto Hänninen, Anne Knol: European Perspectives on Environmental Burden of Disease: Esimates for Nine Stressors in Six European Countries,
Authors and National Institute for Health and Welfare (THL), Report 1/2011 [1] [2] Cite error: Invalid
<ref>tag; name "EBoDe" defined multiple times with different content Cite error: Invalid<ref>tag; name "EBoDe" defined multiple times with different content