Odour
| [show] This page is a encyclopedia article.
The page identifier is Op_en3725 |
|---|
Katleen De Brouwere and Rudi Torfs, VITO
Introduction
Odour is perceived by our brains in response to chemicals present in the air we breathe. Most of the environmental odours are a mixture of many chemicals (odorants) at very low concentrations. Odours are caused by the presence of (certain) chemicals in air (for example volatile organic compounds, VOCs). The investigation of the chemical toxicity as such is out of the scope of this scoping note. For most odours/chemicals, thresholds for the chemical toxicity are at much higher levels than the threshold of the corresponding odour detection, and also the threshold of odour annoyance and irritation.
Relevant exposure metrics
A standardized approach to express odour concentrations is in terms of Odour Units (OU/m³). The number of OUs in a sample represents the number of times the odorous gas must be diluted with odour-free air to reach the point where it elicits a response from just 50 % of the population. Thus, when an odour is present at a level of 1 OU, the concentration is equal to that of the threshold.
However, this exposure metric merely expresses the intensity of an odour, and does not acknowledge for the (un)pleasantness of the odour, called ‘the hedonic tone’. The hedonic tone depends on the chemical composition of the odorant and this factor appeared to play an important role in the dose-response function of odour (Sucker et al., 2007). Methods have been developed to assess the hedonic tone of odours (e.g. Both et al., 2004).
Two mean categories are available to assess odours: sensory and chemical techniques. Sensory techniques (e.g. olfactometry) utilise human assessors to assess odour. The advantage of sensory methods is that they provide a direct link to how odours are perceived by humans. This is very useful for studies that involve assessment of annoyance or health effects. In addition to the assessment of ‘total odour’ by sensory techniques, sensory techniques also exist for assessment of odour character, intensity and hedonic tone. Some techniques like olfactometry which utilise a panel of trained noses to assess odour, make it possible to express odour in standardized units. However, in more complaint-based or epidemiological studies, odour perception is less quantitatively described. In such studies, assessors for odour are more of a qualitative, describing and categorized kind. Chemical methods use conventional analytical techniques (gas chromatography, mass spectroscopy, wet chemical analyses and electronic noses). Disadvantage of chemical techniques is that they do not reflect the intensity of odours as experienced by humans.
Sensory methods are generally preferred to chemical methods in studies investigating dose-response effects.
Health effects of short-term and long - term exposures
A division between short-term and long-term exposure is not very relevant; what is more relevant is the odour-specific discussion on dose-response (psychological effects) which apply for both short and long term exposure. At the end of this section, a paragraph is devoted specifically to long-term exposure.
Historically, unpleasant odours have been considered as a warning sign of indicators of potential health risk to human health, but not necessarily as direct triggers of health effects. Thus, malodours provide warnings of microbial growth in food, gas leaks, fires and unsanitary conditions. More and more, public awareness has recently raised that, beyond this warning function of odours, odour sensations themselves may cause health symptoms (Shiffman and Williams, 2005).
Levels of odour exposure, and corresponding effects are, in the following order (Schiffman and Williams, 2005):
- odour detection
- odour recognition
- odour annoyance
- odour intolerance (causing somatic effects)
- perceived irritant
- somatic irritant
- chronic toxicity
- acute toxicity
WHO defined ‘health’ in 1968 as ‘health is an incomplete state of physical, mental and social well-being, and not merely the absence of disease or infirmity’. According to this definition, effects starting from annoyance and intolerance in the above list should also be considered as a ‘health effect’. Indeed, annoyance and irritation are very often recorded as an effect of elevated, unpleasant odour levels (Sucker et al. 2007). Further, according to Schiffman and Williams (2005), effects 7 & 8 (chronic and acute toxicity) should be not be considered as an odorant effect but rather a compound with toxic effects that happens to have an odour (cfr. also the delineation of this scoping note in the introduction).
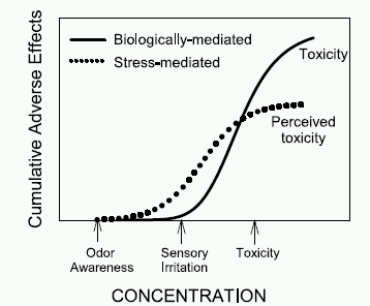
Traditional toxicological models are not suitable to describe a dose-response relationship between odour exposure and health effects. Some odorous compounds produce somatic symptoms, at concentrations (sometimes far) below toxicological thresholds, and for these effects, non-toxicological mechanisms explain the effects. Such explanations are given by biopsychosocial or psychophysical models (e.g. Smeets et al, 2005, Dalton, 2003). In such models, the interaction between psychological factors (stress) induced by odour perception and purely biologically toxicology response is illustrated (Figure 1 source: Dalton, 2003). Perceived toxicity starts earlier on the dose-response curve than purely biologically mediated toxicity, because the odour awareness induces stress, irritation and other annoyances.
Shusterman (1999) explained some of the odour influenced health responses by: 1) innate odour aversion, 2) odour-related exacerbation of underlying conditions, 3) odour-related aversive conditioning, and 4) odour-related, stress-induced illness. The focus of this scoping note is on the health effects (including annoyance, irritation) of odorants seen at exposures below biologically-mediated toxicological (acute and chronic exposure) toxic thresholds for the substance with odorant properties. This delineation is important to draw because we do not want to give the impression that the health effects listed here are the only health effects caused by substances producing odorants. For example, volatile organic compounds (xylenes, naphthalene, pinene, benzene, toluene,…) above biologically-mediated toxicological thresholds) are cause of health effects such asthma, respiratory symptoms, cancer,… These are substance-specific effects, not caused by the odorants properties of the substance, and thus out of the scope of ‘odour’. What is envisaged here is the health effect of the odour in se. Nevertheless, it is recognized that odours with different hedonic tones exist (depending to some extent on the property of the substance), and will also produce to a different extend health effects (Sucker, 2007).
Somatic complaints due to odour exposure are symptoms such as irritation, annoyance, headache, nausea and shortness of breath, and other injuries of respiratory organs and nose (Shusterman, 1992, 1999)
Figure 1: Hypothetical functions illustrating the cumulative adverse symptoms response to chemicals possessing both odour, irritant and toxicity properties (source: Dalton, 2003).
Nimmermark (2004) reviewed symptoms due to odour complaints reported by residents in the vicinity of animals production facilities. The following symptoms were recorded:
- symptoms on nose: irritation in nose,
- symptoms on eyes: irritation in eyes,
- symptoms on throat,
- respiratory symptoms: irritation in throat, breathing problems, chest tightness, cough,
- symptoms on skin: skin irritation,
- symptoms on head: headache,
- gastric symptoms: diarrhoea, and
- mental symptoms: tiredness, weakness, less vigour, confusion, depression, tension, anger, sleeping difficulties, annoyance and reduced quality of life.
According to Nimmermark (2004), the protection system triggered by the trigeminal nerve system prevents severe effects.
The above described effects pertain both to short-term and long-term exposures. Major part of the odour-related health effects studies are based on complaints recorded among persons living in the neighbourhood of odour emitting facilities (animal farms, sludge facilities, …) and thus pertain to long-term exposure. However, the same effects occur also for short-term exposure. Persons exposed for a short-term or intermediate to odours are in many cases even more susceptible to odours, have a lower odour detection threshold than people with frequent previous or long term exposure.
A possible health effect of long-term exposure is the loss of olfactory function. This phenomena has been reported in the past (e.g. Hirsch et al., 1999, Naus et al., 1968, and Emmet et al. 1976, the latter two references cited in Cone and Shusterman, 1991) though mainly based on effects seen after occupational exposure to odours.
What health endpoints might be quantified?
The major part of the (less recent) literature has described odour – health dose-response relationships in a qualitative way, neither with quantification of the exposure (odour) nor with quantification of the effects. For example, the vicinity of animal farms has been frequently used as a proxy for ‘odour’ and the prevalence of effects such as irritation have been reported in terms of ‘absence or presence of irritation’ (Nimmermark, 2004). Most of these studies do neither give any information about the intensity, duration or hedonic tone nor about the severity or frequency of the health effects.
However, some recent studies (e.g. Avery et al., 2004; Sucker et al,, 2007) are moving in the way forward to enable quantification of odour – health quantifiable relationships. In the study of Sucker et al. (2007), both 1) the severity of effects (annoyance and frequency of somatic effects) among the residents in the vicinity of odour sources and 2) the odour perception (odour exposure and hedonic tone) was quantified. Odour perception was measured using standard protocols and trained and calibrated observers (panellists). Quantified dose – effects relations were derived by Sucker et al. (2007). For example, hedonic tone (Odds ratio (OR) = 4.9 ; 95 % C.I.: 3.4-7.2) had the largest effect on % annoyed persons, followed by the odour frequency (OR = 1.6; 95 % C.I.: 1.3-2.0) and intensity (OR = 1.3; 95 % C.I.: 1.1- 1.5). Avery et al. (2004) quantified the effect of odour intensity on secretory immunoglobulin (sIgA) in adults living in the neighbourhood of industrial hog farming operations. the ln(sIgA) concentration declined on average 0.058 (0.032) for each incremental 1-unit increase in reported odour from 4 to 9 (on a 9 point scale for odour), suggesting reduced levels of sIgA in response to moderate or high odour.
Albeit, such studies are rather scarce, and there is still a long way to reach universal, widely applicable quantitative odour – health dose response functions.
Further, it should be kept in mind that dose-response models for odour are generally not linear. For example, if the concentration of the odour is decreased by a given factor, the fraction of the population that responds to the odour does not necessarily decrease by the same factor (Nicell, 2003). The same observation can be made for other characteristics such as odour intensity, and also on individual level, the response of a individual to increasing odour concentrations is unlikely to be linear.
Is there evidence of a threshold or ‘safe’ level of odour ?
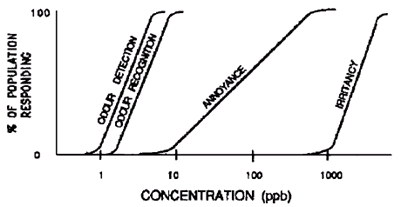
YES and NO: Yes, there are thresholds for ‘odour detection‘, and in general, annoyance, irritation and more severe health effects do not start before the odour detection and odour recognition threshold (see Figure 2). However, in some cases, irritation starts at exposures below the odour detection limit. In these cases, it is the rather the health effect caused by the toxic properties of the odorant itself than the odour itself which causes the health effect.
Figure 2: the odour – impact model, as illustrated for hydrogen sulphide (source: Shusterman, 1999. Moreover, odour thresholds (either thresholds for detection, annoyance or irritation) are determined by the hedonic tone of the odour (Nicell et al., 2003).
What sub-groups of the population are most susceptible or otherwise will need special consideration in quantification?
The major part of studies investigating odour related health effects is focused on healthy adults. There is however within the population a rather wide variance on sensitivity to odour irritation.
Many people with asthma identify odorants that specifically worsen their asthma (Cone and Shusterman, 1991). Therefore, asthma patients could be considered as a group requiring special consideration in quantification. The types of odorants associated with worsening of asthma include flowers, insecticide, perfumes, household cleaners, cooking, cigarettes, auto exhaust, paint vapors, and body odor). The mechanism of odorant-associated asthma is not clear.
References
- Avery, R.C., Wing, S., Marshall, S.W., Schiffman, S.S. 2004. Odor from industrial hog farming operations and mucosal immune function in neighbors. Archives of Environmental Health, 59(2): 101-108.
- Both, R., Sucker, K., Winneke, G., Koch, E. 2004. Odour intensity and hedonic tone – important parameters to describe odour annoyance to residents? Water Science and Technology, 50(4): 83-92.
- Cone, E., Shuterman, D. 1991. Health effects of indoor odorants. Environmental Health Perspectives, 95: 53-59.
- Dalton P., 2003. Upper airway irritation, odor perception and health risk due to airborne chemicals. Toxicology Letters, 140-141: 239-248.
- Hirsch, A., Zavala, G. 1999. Long-term effects on the olfactory system of exposure to hydrogen sulphide. Occup. Environ. Med., 56: 284-287.
- Nicell, J.A. 2003. Expressions to relate population response to odour concentration. Atmospheric Environment, 37: 4955-4964.
- Nimmermark, S. 2004. Odour influence on well-being and health with specific focus on animal production emissions. Ann. Agric. Environ. Med., 11: 163-173.
- Schiffman, S.S., Williams, C.M. 2005. Science of odor as a potential health issue. J. Environ. Qual., 34: 129-138.
- Shusterman, D. 1992. Critical Review: the health significance of environmental odor pollution. Arch. Environ. Health, 47: 76-87.
- Shusterman, D. 1999. The health significance of environmental odor pollution: revisited. Journal of Environmental Medicine, 1: 249-258.
- Smeets, M.A.M., Dalton, P.H. 2005. Evaluating the human response to chemicals: odor, irritation and non-sensory factors. Environmental Toxicology and Pharmacology, 19: 581-588.
- Sucker, K., Both, R., Bisschoff, M., Guski, R., Krämer,U., Winneke, G. 2007. Odor frequency and odor annoyance part II: dose-response associations and their modification by hedonic tone. Int. Arch. Occup. Environ. Health. DOI 10.2007/s00420-007-0262-4.